NCP Nursing Care Plan for Acute Respiratory Failure. When the lungs can't adequately maintain arterial oxygenation or eliminate carbon dioxide (CO2), acute respiratory failure occurs. If not checked and treated, the condition leads to tissue hypoxia. In patients with essentially normal lung tissue, acute respiratory failure usually produces a partial pressure of arterial CO2 (PaCO2) greater than 50 mm Hg and a partial pressure of arterial oxygen (PaO2) less than 50 mm Hg.
These limits, however, don't apply to patients with chronic obstructive pulmonary disease COPD.
Causes for Acute Respiratory Failure
Acute respiratory failure may develop from COPD, Other causes of acute respiratory failure include:
- Central nervous system depression due to head trauma or injudicious use of sedatives, opioids, tranquilizers, or oxygen
- Cardiovascular disorders (myocardial infarction, heart failure, or pulmonary emboli)
- Airway irritants, such as smoke or fumes
- Endocrine or metabolic disorders, such as myxedema or metabolic acidosis
- Thoracic abnormalities, such as chest trauma, pneumothorax, or thoracic or abdominal surgery
- Noncompliance with prescribed bronchodilator or corticosteroid therapy.
Complications for Acute Respiratory Failure
- Tissue hypoxia,
- Metabolic acidosis.
- Respiratory and cardiac arrest.
Nursing Assessment Nursing Care Plan for Acute Respiratory Failure
- Inspection, note cyanosis of the oral mucosa, lips, and nail beds; nasal flaring; and ashen skin. You may observe the patient yawning and using accessory muscles to breathe. He may appear restless, anxious, depressed, lethargic, agitated, or confused. Additionally, he usually exhibits tachypnea, which signals impending respiratory failure.
- Palpation may reveal cold, clammy skin and asymmetrical chest movement, which suggests pneumothorax. If tactile fremitus is present, notice that it decreases over an obstructed bronchi or pleural effusion but increases over consolidated lung tissue.
- Percussion especially in patients with COPD reveals hyperresonance. If acute respiratory failure results from atelectasis or pneumonia, percussion usually produces a dull or flat sound.
- Auscultation typically discloses diminished breath sounds. In patients with pneumothorax, breath sounds may be absent. In other cases of respiratory failure, you may hear such adventitious breath sounds as wheezes and rhonchi . If you hear crackles, suspect pulmonary edema as the cause of respiratory failure.
Diagnostic tests for Acute Respiratory Failure
- ABG analysis
- Chest X-rays
- Electrocardiography (ECG)
- Pulse oximetry.
- Blood tests such as a white blood cell count low hematocrit and decreased hemoglobin levels signal blood loss, which indicates decreased oxygen-carrying capacity.
- Serum electrolyte
- Pulmonary artery
- Blood culture and sputum culture to identify the pathogen.
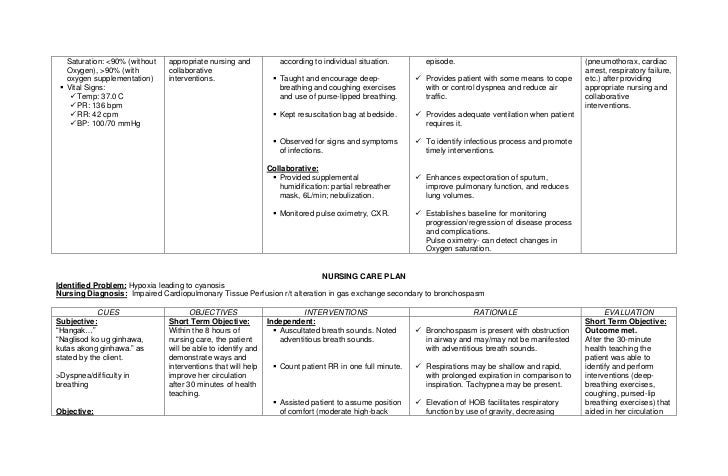
Nursing diagnosis Nursing Care Plan for Acute Respiratory Failure
Common Nursing diagnosis found in patient with Acute Respiratory Failure
- Anxiety
- Decreased cardiac output
- Fatigue
- Fear
- Impaired gas exchange
- Impaired physical mobility
- Impaired verbal communication
- Ineffective airway clearance
- Ineffective coping
- Ineffective tissue perfusion: Cardiopulmonary
- Risk for impaired skin integrity
- Risk for infection
Nursing outcomes Nursing Care Plan for Acute Respiratory Failure
Patient will :
- Express feelings of reduced anxiety.
- Remain hemodynamically stable.
- Verbalize the importance of balancing activity with adequate rest periods.
- Discuss fears or concerns.
- Maintain adequate ventilation and oxygenation
- Maintain joint range-of-motion and muscle strength.
- Use alternate means of communication.
- Maintain a patent airway.
- Use support systems to assist with coping.
- Maintain adequate cardiopulmonary perfusion.
- Maintain skin integrity.
- Remain free from signs or symptoms of infection.
Nursing Interventions Nursing Care Plan for Acute Respiratory Failure
- Anxiety Reduction: Minimizing apprehension, dread, foreboding, or uneasiness related to an unidentified source or anticipated danger
- Calming Technique: Reducing anxiety in patient experiencing acute distress
- Hemodynamic Regulation: Optimization of heart rate, preload, afterload, and contractility
- Cardiac Care: Limitation of complications resulting from an imbalance between myocardial oxygen supply and demand for a patient with symptoms of impaired cardiac function
- Circulatory Care: Mechanical Assist Devices: Temporary support of the circulation through the use of mechanical devices or pumps
- Energy Management: Regulating energy use to treat or prevent fatigue and optimize function
- Exercise Promotion: Facilitation of regular physical exercise to maintain or advance to a higher level of fitness and health
- Nutrition Management: Assisting with or providing a balanced dietary intake of foods and fluids
- Anxiety Reduction: Minimizing apprehension, dread, foreboding, or uneasiness related to an unidentified source or anticipated danger
- Security Enhancement: Intensifying a patient’s sense of physical and psychological safety
- Coping Enhancement: Assisting a patient to adapt to perceived stressors, changes, or threats that interfere with meeting life demands and roles
- Respiratory Monitoring: Collection and analysis of patient data to ensure airway patency and adequate gas exchange
- Oxygen Therapy: Administration of oxygen and monitoring of its effectiveness
- Airway Management: Facilitation of patency of air passages
- Exercise Therapy: [specify]: Use of active or passive body movement to maintain or restore flexibility; use of specific activity or exercise protocols to enhance or restore controlled body movement, etc.
- Pain Management: Alleviation of pain or a reduction in pain to a level of comfort acceptable to the patient
- Communication Enhancement: Speech Deficit: Assistance in accepting and learning alternative methods for living with impaired speech
- Communication Enhancement: Hearing Deficit: Assistance in accepting and learning alternative methods for living with diminished hearing
- Active Listening: Attending closely to and attaching significance to a patient’s verbal and nonverbal messages
- Airway Management: Facilitation of patency of air passages
- Respiratory Monitoring: Collection and analysis of patient data to ensure airway patency and adequate gas exchange
- Cough Enhancement: Promotion of deep inhalation by the patient with subsequent generation of high intrathoracic pressures and compression of underlying lung parenchyma for the forceful expulsion of air
- Coping Enhancement: Assisting a patient to adapt to perceived stressors, changes, or threats that interfere with meeting life demands and roles
- Decision-Making Support: Providing information and support for a person who is making a decision regarding healthcare
- Fluid/Electrolyte Management: Promotion of fluid/electrolyte balance and prevention of complications resulting from abnormal or undesired fluid/serum electrolyte levels
- Cerebral Perfusion Promotion: Promotion of adequate perfusion and limitation of complications for a patient experiencing or at risk for inadequate cerebral perfusion
- Cardiac Care: Limitation of complications resulting from an imbalance between myocardial oxygen supply and demand for a patient with symptoms of impaired cardiac function
- Circulatory Care: Arterial/Venous Insufficiency: Promotion of arterial/venous circulation
- Skin Surveillance: Collection and analysis of patient data to maintain skin and mucous membrane integrity
- Pressure Management: Minimizing pressure to body parts
- Pressure Ulcer Prevention: Prevention of pressure ulcers for a patient at high risk for developing them
- Infection Protection: Prevention and early detection of infection in a patient at risk
- Infection Control: Minimizing the acquisition and transmission of infectious agents
- Surveillance: Purposeful and ongoing acquisition, interpretation, and synthesis of patient data for clinical decision making