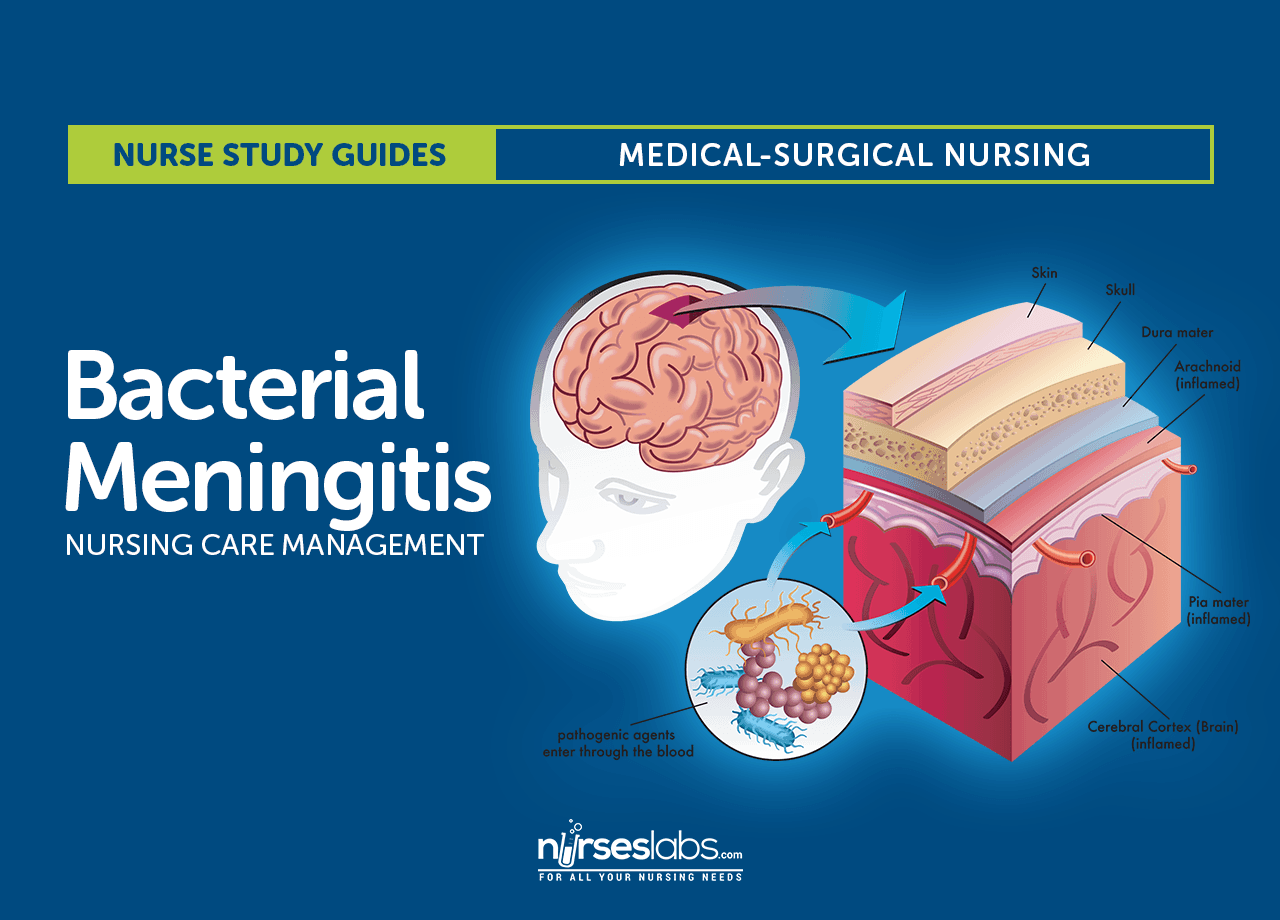
NCP Nursing Care Plans For Meningococcal Infections. Two major meningococcal infections, meningitis and meningococcemia, are caused by the gram-negative bacteria Neisseria meningitidis, which also causes primary pneumonia, purulent conjunctivitis, endocarditis, sinusitis, and genital infection. Meningococcemia occurs as simple bacteremia, fulminating meningococcemia and, rarely, chronic meningococcemia. It commonly accompanies meningitis. Meningococcal infections may occur sporadically or in epidemics; particularly virulent infections may be fatal within a matter of hours.
Causes For Meningococcal Infections
Neisseria meningitidis has seven serogroups (A, B, C, D, X, Y, and Z
Complications For Meningococcal Infections
- Respiratory failure that requires mechanical ventilation. If severe
- Disseminated intravascular coagulation (DIC) develops,
- Hemorrhage GI tract, and urinary tract, as well as tissue ischemia.
- Septic arthritis, pericarditis, or endophthalmitis.
- Aspiration of the organism can cause meningococcal pneumonia.
- Meningococcal infections may progress very rapidly, causing neurologic deterioration and even death.
Nursing Assessment Nursing Care Plans For Meningococcal Infections
Features of meningococcal bacteremia include sudden spiking fever, headache, sore throat, cough, chills, myalgia , arthralgia, tachycardia, tachypnea, mild hypotension, and a petechial, nodular, or maculopapular rash. Headache and stiff neck can also occur as the infection extends to the meninges.
Characteristics of the rare chronic meningococcemia include intermittent fever, rash, joint pain, and an enlarged spleen.
Diagnostic tests For Meningococcal Infections
• Blood culture,
• Cerebrospinal Fluid CSF culture
Nursing diagnosis Nursing Care Plans For Meningococcal Infections
- Acute pain
- Hyperthermia
- Decreased cardiac output
- Impaired skin integrity
- Ineffective breathing pattern
- Ineffective tissue perfusion: Cardiopulmonary
Nursing outcomes Nursing Care Plans For Meningococcal Infections
- The patient will express feelings of comfort and relief from pain.
- The patient will maintain adequate cardiac output.
- The patient will remain a febrile.
- The patient's skin will remain warm, dry, and intact.
- The patient will exhibit healed or improved lesions or wounds.
- The patient's ventilation will remain adequate.
- The patient will maintain collateral circulation.
- The patient will remain hemodynamically stable.
Nursing interventions Nursing Care Plans For Meningococcal Infections
- Pain Management: Alleviation of pain or a reduction in pain to a level of comfort that is acceptable to the patient
- Analgesic Administration: Use of pharmacologic agents to reduce or eliminate pain
- Temperature Regulation: Attaining and/or maintaining body temperature within a normal range
- Fever Treatment: Management of a patient with hyperpyrexia caused by non environmental factors
- Malignant Hyperthermia Precautions: Prevention or reduction of hyper metabolic response to pharmacological agents
- Hemodynamic Regulation: Optimization of heart rate, preload, after load, and contractility
- Cardiac Care: Limitation of complications resulting from an imbalance between myocardial oxygen supply and demand for a patient with symptoms of impaired cardiac function
- Skin Surveillance: Collection and analysis of patient data to maintain skin and mucous membrane integrity
- Pressure Management: Minimizing pressure to body parts
- Pressure Ulcer Prevention: Prevention of pressure ulcers for a patient at high risk for developing them
- Ventilation Assistance: Promotion of an optimal spontaneous breathing pattern that maximizes oxygen and carbon dioxide exchange in the lungs
- Airway Management: Facilitation of patency of air passages
- Respiratory Monitoring: Collection and analysis of patient data to ensure airway patency and adequate gas exchange
- Fluid/Electrolyte Management: Promotion of fluid/electrolyte balance and prevention of complications resulting from abnormal or undesired fluid/serum electrolyte levels
- Cerebral Perfusion Promotion: Promotion of adequate perfusion and limitation of complications for a patient experiencing or at risk for inadequate cerebral perfusion
- Cardiac Care: Limitation of complications resulting from an imbalance between myocardial oxygen supply and demand for a patient with symptoms of impaired cardiac function
- Gastrointestinal Intubation: Insertion of a tube into the gastrointestinal tract Circulatory Care: Arterial/Venous Insufficiency: Promotion of arterial/venous circulation